Unraveling the Power of AI in Corneal Diagnosis and Treatment
Authors: Lopes, B.T., Eliasy, A., and Ambrosio, R.
Journal: Current Ophthalmology Reports
Publication Date: Jul 2019
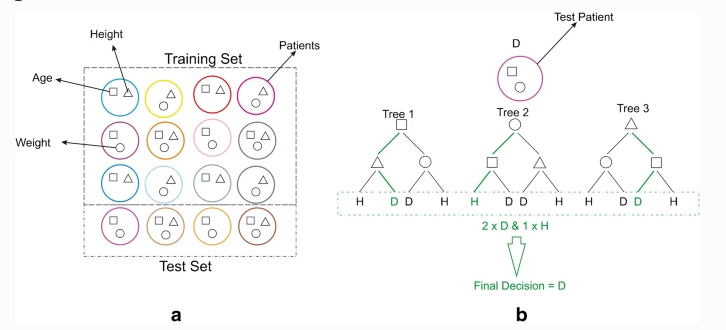
Example of a random forest model. a - The patients included in the train and test sets, for exemplification purposes, different characteristics of height, age, and weight are graphically expressed with geometrical shapes (triangle, square, and circle, respectively). b - A very simple random forest model composed of 3 trees trained with the three characteristics to separate healthy (H) and diseased (D) and the classification path (in green) of a new patient
Summary:
The field of ophthalmology, particularly the cornea subspecialty, has always been at the forefront of using technology to improve the diagnosis and treatment of eye diseases. In our research, we have explored the potential of artificial intelligence (AI) techniques and models to enhance clinical decisions for patients with corneal diseases and conditions.
The advancements in corneal imaging devices have led to a wealth of information that can be crucial for early disease detection. However, this information overload can hamper decision-making. AI models are perfectly suited to address this challenge by efficiently analyzing data to support clinical decisions.
Our findings indicate that AI models are already in use by clinicians for refractive surgery screening. The challenge now is to coordinate multicentre collaborations to build high-quality and large data collections to train and improve AI models. AI has numerous potential applications for ophthalmologists, ultimately empowering them to make better clinical decisions.
In our research, we've also observed how AI has benefitted in vivo corneal morphology exams, with neural networks being used to automatically identify healthy corneal layers on confocal microscopy exams. Furthermore, AI has been used in the assessment of corneal biomechanics, providing a simple output parameter that can be directly used as a risk profiling tool.
Additionally, AI has been applied in corneal surgery, such as haze and demarcation line quantification after cross-linking surgery, as well as graft detachment evaluation in corneal posterior lamellar transplant surgery.
Despite these promising developments, there are still limitations that need to be addressed. Large training sets are required for deep learning, and there are technical challenges in acquiring images and differences between imaging devices. Moreover, high computational power and efficient data sharing systems under strict privacy rules are needed to facilitate AI advancements.
In conclusion, AI models are already available and widely used in refractive surgery screening, with several other applications under rapid development. By collaborating with high-tech companies, gathering large datasets, and implementing efficient data sharing systems, we can improve the accuracy of AI models and expand their applications in corneal diseases.