Mystery of Keratoconic Corneas: A Closer Look at Collagen Fibril Density
Authors: Zhou, D., Abass, A., Lopes, B., Eliasy, A., Hayes, S., Boote, C., Meek, K.M., Movchan, A., Movchan, N., and Elsheikh, A.
Journal: Journal of the Royal Society Interface
Publication Date: Feb 2021
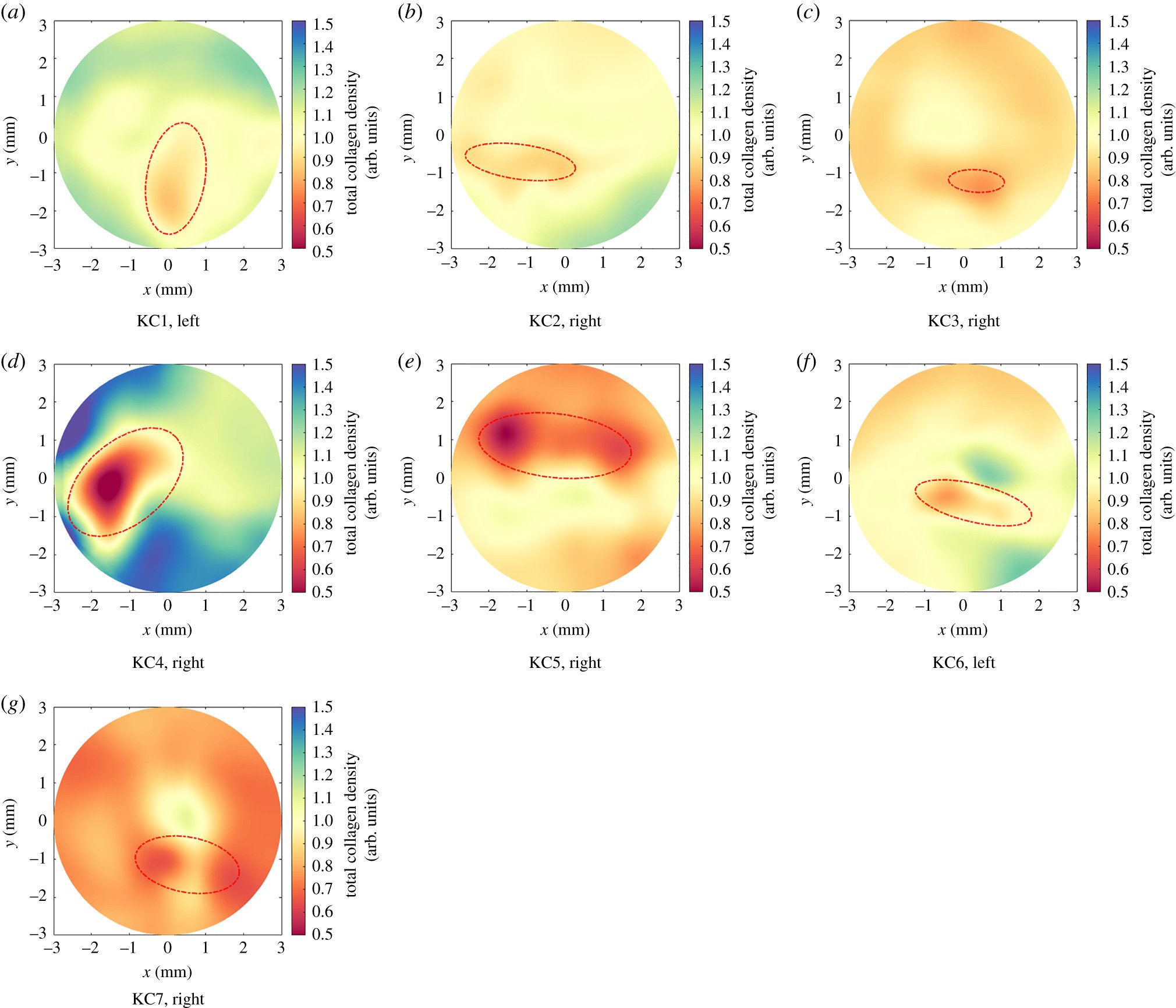
Fibril density maps for seven keratoconic corneas. The origin (0,0) is the corneal apex. Red lines represent the KC cone boundaries.
Summary:
Keratoconus (KC) is a non-inflammatory corneal disease affecting approximately 1 in 2000 individuals. The condition causes the cornea to become thin and develop a cone-shaped protrusion, leading to visual impairment. Although its exact cause remains unknown, researchers have identified that changes in the collagen fibrils within the cornea play a significant role in the development of KC.
In our study, we focused on estimating the reduction in collagen fibril density in the central 6mm radius of keratoconic corneas. We analysed the microstructure and videokeratography data of seven keratoconic and six healthy corneas. Our findings revealed that the collagen fibril density in the cones of keratoconic corneas could be as much as 35% lower compared to healthy corneas.
We also developed a linear approximation to relate the magnitude of reduction to the refractive power, minimum corneal thickness, and cone area. This method can predict the mean fibril density in the cone area of a keratoconic eye, which can be applied in microstructure-based finite-element models to regulate its stiffness level and the stiffness distribution within the areas affected by keratoconus.
Our research showed that the fibril distribution outside the cone areas was not affected by keratoconus development and progression, meaning it was similar to the fibril distribution in healthy corneas. These findings will make it possible to develop customised numerical models to predict the biomechanical behaviour of keratoconic corneas.
Despite its contributions, our study has some limitations, such as the small number of cornea specimens and the inability to include the cone region in our analysis due to low-intensity collagen X-ray scatter. As more data becomes available, the method we've developed will be updated and refined.
In conclusion, our study has provided valuable insights into the reduction of collagen fibril density inside the cone areas of keratoconic corneas and its impact on the biomechanical behaviour of the affected eyes. This research will ultimately help pave the way for more effective diagnosis and treatment options for individuals living with keratoconus.